Delivery of health services is often under-funded. This is not unique to poor countries — from the UK’s travails with the NHS to India’s under-resourced health sector, examples abound of the detrimental impact that an under-funded public health system results in.
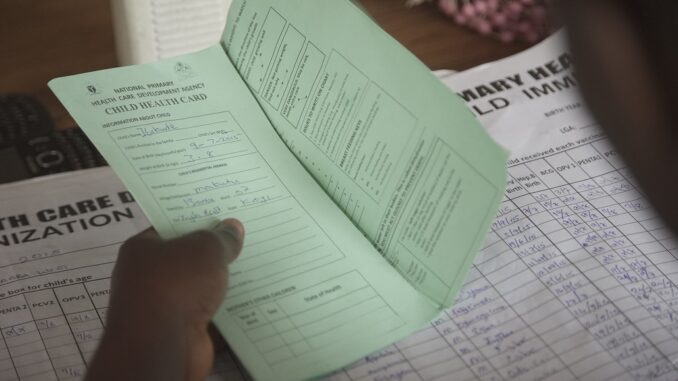
Findings from a recent study in Nigeria (Khanna, M., Loevinsohn, B., Pradhan, E. et al. Decentralized facility financing versus performance-based payments in primary health care: a large-scale randomized controlled trial in Nigeria.) provide insights into the potential benefits of decentralized delivery of health services, when it has access to a predictable financing mechanism. The researchers studied 571 health facilities, which were randomly assigned to two treatment arms — performance-based financing (PBF) and direct facility financing (DFF). The study ran over three years, covering over 9 million people. Facilities that were part of the PBF model received a quarterly amount based on agreed upon service standards. On the other hand, under the DFF, facilities received a fixed quarterly amount that was not linked to specific results.
While the researchers found that both financing modalities had significant effects on the access to and quality of services delivered by the health centers, there was a clear cost advantage to the DFF model. DFF cost half of what PBF did, accounting for the costs of running and supervising the interventions. This is a significant finding that suggests that a decentralized health services model can deliver the same results as a more expensive (and likely, more complex) performance-based model. The authors do point out important caveats in their study, in particular related to the selection of treatment sites and their inability to disaggregate the different components of the interventions being studied.
However, these findings are important in advancing our understanding of service delivery in difficult contexts, and in particular, the importance of adequate financing. Over the years, doubts have been raised on the merits of decentralization itself — on its ability to improve quality of services, raise resources and to enhance local accountability. This study helps discuss some of these questions further, even if rooted in its specific context. Three key areas for discussion emerge:
A well-financed decentralised model is a basic building block: Often in this sector, we spend money designing complex financing mechanisms, but forget the basics. It appears here that gains from financing heath centres to function with better autonomy and financial stability can deliver benefits for the local population. Without adequate funds, decentralisation is a sham. Another study from Cameroon throws up similar results — a PBF approach did not add value to basic financing of facilities. A simple and targeted payment-by-results or a PBF model could yield further benefits, but any such intervention should build on a system that grants greater autonomy to frontline workers, and establish incentives that can genuinely motivate them. The researchers point out that for PBF to work in the first place, outcome indicators must be chosen from services that are ‘’in the health worker’s locus of control.’’
The role of supervision and vertical accountability: Both treatment arms in the Nigeria study benefited from regular supervision, which as the researchers note, even as a standalone intervention, would have a significant impact. In decentralised systems, while we expect local accountability pressures to play a significant role, it should not come at the cost of supervision by officials from ‘above’. This supervision is important to encourage better performance on matters such as regulatory compliance and equity in service provision, as well as to support capacity enhancement through training and mentorship.
Inclusion does not come cheap: More needs to be done to reach the poorest. The Nigeria study found relatively little change in access among the two poorest wealth quintiles across the health facilities. One might assume that in a decentralised service delivery model, the benefits from service delivery will not remain clustered amongst the richer parts of the population. However, without a concerted effort to be more inclusive, elite capture of services is often the reality. This also often occurs in contexts where specific areas of service delivery are decentralised down to the local facilities, but such reform is not accompanied by any meaningful democratic decentralisation. Further efforts need to be directed towards improving local accountability — having people demand access to better services.
Service delivery — in health and education, for instance — is currently decentralized in many parts of the world. Without adequate financing though, it will amount to little. This may seem simple, but remains an oft-forgotten facet in development, where we often rush to design/develop/innovate the next shiny sophisticated solution, sometimes forgetting what’s staring us in the face.
Suvojit Chattopadhyay is a Project Director at Adam Smith International.
Read the original blog—and more blogs from Suvojit Chattopadhyay on Medium.com: https://medium.com/@suvojitc
Photo credit: Sim USA/ Flicker under Creactive Common License (CC BY-SA 2.0).



